Scientists have long known that the APOE4 gene variant is a significant risk factor for Alzheimer’s disease. But until recently, little has been understood about why and how this gene causes brain damage. That may be changing, thanks to a new study conducted by neuroscientist Li-Huei Tsai and a team of colleagues at the Massachusetts Institute of Technology (MIT) in Cambridge using transgenic mouse models.
APOE4 and Alzheimer’s
The APOE gene codes for a protein called apolipoprotein E, which assists with the transportation and metabolism of fats in the body. It is also involved in the repair and maintenance of nerve tissue. There are three main variants of the APOE gene: APOE2, APOE3, and APOE4.
People who carry one copy of the APOE4 variant are at an increased risk of developing Alzheimer’s disease, a progressive brain disorder that causes cognitive decline and memory loss. Carrying the APOE4 gene is one of the most significant risk factors for Alzheimer’s disease. This risk is even greater for people who carry two copies of the APOE4 variant.
However, it is important to note that the presence of the APOE4 variant is not the only factor that contributes to the development of Alzheimer’s disease, and many people with the APOE4 variant never develop the condition.
Research has shown that the APOE4 variant may affect the brain in several ways that could increase the risk of Alzheimer’s disease. For example, it has been found to increase the production of amyloid beta, a protein that accumulates in the brains of people with Alzheimer’s and is thought to play a role in the development of the disease. APOE4 may also disrupt the clearance of amyloid beta from the brain, leading to its accumulation. The APOE4 variant has been found to alter the structure and function of neurons in the brain, which could contribute to cognitive decline.
Transgenic Mouse Models and APOE4: A Breakthrough
The fact that APOE4 increases the risk of Alzheimer’s disease has been thoroughly studied, but until recently, researchers struggled to understand why APOE4 has this adverse effect. Li-Huei Tsai and her team’s research with transgenic mouse models are finally shining a light on a previously murky subject.
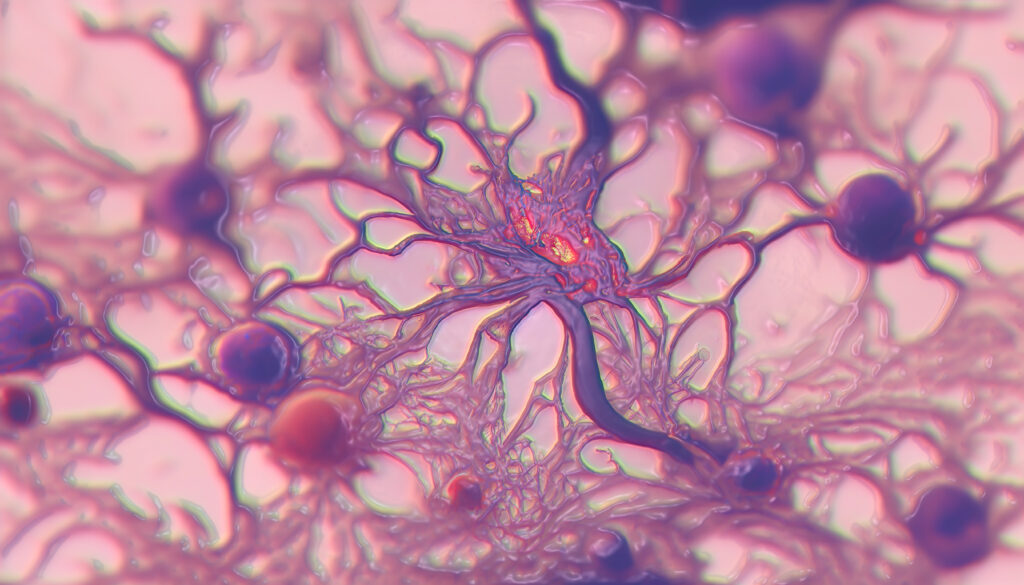
The study, published in Nature, found that APOE4 triggers cholesterol accumulation in oligodendrocytes, a type of brain cell. This overproduction of cholesterol damages the oligodendrocytes’ ability to coat nerve fibers with myelin, a fatty, protective substance that insulates nerve fibers and improves the speed and efficiency of nerve impulse conduction. With this ability damaged, the brain’s electrical signaling slows, and cognition declines.
Previous research has indicated that APOE4 in Alzheimer’s patients may be related to problems with brain cells’ ability to process fats, or lipids. Confirming this in their research, Tsai and her team found lipid metabolizing abnormalities in brain cells affected by APOE4. But the team noted that in the brain tissue of Alzheimer’s patients, one defect – the way that oligodendrocytes processed cholesterol – was particularly extreme.
Treatment Implications
Using transgenic mouse models, Tsai and her team treated APOE4-carrying cells with cyclodextrin, a drug that stimulates the removal of cholesterol. The results were striking. Not only did cyclodextrin treatment help to restore myelin function, but for mouse models with two APOE4 copies, the cyclodextrin treatment appeared to flush cholesterol from the brain, improve the flow of cholesterol into myelin sheaths, and boost cognition.
The transgenic mouse model findings are in line with a previous single-subject experimental human study, wherein a person with Alzheimer’s experienced cognitive improvements after being treated with a special access formulation of cyclodextrin. However, researchers caution that cyclodextrin treatment has limitations. “It’s kind of sledgehammer,” says Leyla Akay, a neuroscientist in Tsai’s lab and a co-author of the latest study. “It just depletes cholesterol from cells.”
Still, Tsai’s research further highlights the importance of cholesterol accumulation on cognitive functioning and provides critical insight into causes and potential future treatments for Alzheimer’s disease.
Scantox is a part of Scantox, a GLP/GCP-compliant contract research organization (CRO) delivering the highest grade of Discovery, Regulatory Toxicology and CMC/Analytical services since 1977. Scantox focuses on preclinical studies related to central nervous system (CNS) diseases, rare diseases, and mental disorders. With highly predictive disease models available on site and unparalleled preclinical experience, Scantox can handle most CNS drug development needs for biopharmaceutical companies of all sizes. For more information about Scantox, visit www.scantox.com.