Rare genetic diseases such as ataxia-telangiectasia (A-T) pose significant challenges in the field of medicine. But a new groundbreaking study conducted by researchers at the Korea Advanced Institute of Science and Technology (KAIST) has unveiled a promising new method for using antisense oligonucleotides to treat A-T. Researchers hope that this revolutionary approach will provide treatment options not only for patients with A-T, but also for patients with one of the many rare genetic conditions previously considered untreatable as well as more common diseases like Alzheimer’s disease and Parkinson’s disease.
Roadblocks to Treating Rare Genetic Diseases
About 1 in 10 people across the globe have a rare genetic disease. While having one of these diseases may not be rare, available treatments are. Rare genetic diseases include over 7,000 separate conditions, and only five percent of these diseases have treatments available. For some rare genetic diseases, the road to a diagnosis itself can be complicated and time-consuming. But even with a diagnosis, patients face a serious obstacle: most rare genetic diseases do not have an available treatment.
The absence of effective therapies for rare diseases stems from a complicated combination of factors. Developing tailor-made treatments for these complex conditions demands a comprehensive grasp of each individual patient’s unique genetic variations. Unfortunately, most existing healthcare systems are primarily structured around finding broadly applicable treatments for more common diseases with standard pathologies. For the 1 in 10 people worldwide with a rare disease, most have no treatment options available. This is sobering news, especially for patients with diseases like ataxia-telangiectasia (A-T), a rare, debilitating, and often fatal inherited childhood neurological disease caused by mutations in the ATM (ataxia-telangiectasis mutated) gene. But a groundbreaking new study from KAIST researchers could signal a breakthrough.
Antisense Oligonucleotides to Treat A-T
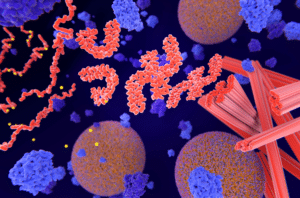
Antisense oligonucleotides, or ASOs, are “short sequences of synthetic nucleic acids, a chain of nucleotides adenine (A), cytosine (C), guanine (G) and thymine (T), connected in a specific sequence.” The term “antisense” refers to the fact that ASOs complement target RNA sequences by binding with them and thus altering their function. But while previous research has indicated that splice-switching ASOs could be a safe and effective treatment option to restore protein levels in certain rare diseases, research progress has been impeded by the lack of a reliable, systematic framework for identifying individuals who would be amenable to this treatment.
This was the first problem the team of KAIST researchers set out to solve for patients with A-T. To do so, the team first conducted whole-genome sequencing analyses on 235 individuals diagnosed with A-T. With this data, the team was able to develop a robust predictive taxonomy that allowed the researchers to assess how amenable each individual might be to splice-switching ASO treatment. This taxonomy allowed the research team to identify 35 individuals (out of the cohort of 235) with ASO-amenable variants.
With this data, the team designed and tested ASOs to target and correct mis-spliced RNA in tissue samples from those 35 patients. One of the ASOs created as part of this process was then administered to a child with A-T, as part of a pilot first-in-human investigational trial. Thus far, this clinical trial has demonstrated good treatment tolerability for the three years that it has been in process.
Results and Future Implications
More than one hundred ASOs are currently at different stages of research in clinical trials, with hundreds more in development. ASOs have treatment potential not only for rare genetic diseases but also for Alzheimer’s disease, Parkinson’s disease, rheumatoid arthritis, and many types of cancer.
The study highlights the potential of using genome sequencing and analysis to identify genetic variants that might respond well to interventions using ASOs. This approach is currently still in the investigational phase, with more research needed to better understand both the risks in a clinical context, as well as to address any logistical, economic, and ethical considerations that may arise. But the research team is hopeful that this study could provide a meaningful framework that could help accelerate the development of individualized ASOs not only for A-T, but for a wide range of diseases previously considered untreatable.
Scantox is a part of Scantox, a GLP/GCP-compliant contract research organization (CRO) delivering the highest grade of Discovery, Regulatory Toxicology and CMC/Analytical services since 1977. Scantox focuses on preclinical studies related to central nervous system (CNS) diseases, rare diseases, and mental disorders. With highly predictive disease models available on site and unparalleled preclinical experience, Scantox can handle most CNS drug development needs for biopharmaceutical companies of all sizes. For more information about Scantox, visit www.scantox.com.