Recent research conducted by MIT scientists may shed light on the involvement of lateral mammillary body neurons in the early stages of Alzheimer’s disease (AD). Researchers found that these neurons exhibit hyperactivity and are more susceptible to neurodegeneration, highlighting their potential role in the onset of cognitive decline. Using a mouse model, the team demonstrated the potential efficacy of reversing memory loss by treating hyperactivity and neurodegeneration with an epilepsy drug. This breakthrough highlights potential new avenues for drug development and therapeutic interventions that could potentially delay cognitive decline in AD patients.
Early Stages of Alzheimer’s Disease
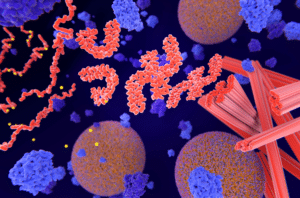
Alzheimer’s disease is a devastating neurodegenerative disorder with no known cure. When a person develops AD, atypical accumulation of the beta-amyloid protein occurs in the brain, causing plaques to build up between neurons, impairing cellular function. The accumulation of beta-amyloid plaques is a hallmark of the early stages of AD, but the exact role that beta-amyloid proteins play both in typical brain function and in the development and progression of AD remains unclear. Indeed, scientists’ understanding of the neural circuits that govern the initiation and progression of AD is incomplete.
Previous studies using 5xFAD mouse models have shown that the mammillary body (MB) in the hypothalamus is one of the first regions of the brain where amyloid deposits can be observed. But until recently, researchers have not known whether there was any relationship between the circuitry of MB neurons and the development of neurodegeneration and memory loss in AD. A new study from MIT could change that.
Pinpointing Neurons in Alzheimer’s Disease
In 2019, Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory, former MIT postdoc Wen-Chin (Brian) Huang, and others conducted a study that found that, in mouse models of AD, the highest concentration of amyloid-beta plaques could be found in the lateral mammillary bodies (MB), subcortical nodes on the underside of the hypothalamus.
Now, Tsai and Huang — along with co-lead authors Zhuyu (Verna) Peng and Mitchell Murdock — have published a new study that has identified a specific set of neurons within the MB that appears most susceptible to hyperactivity, neurodegeneration, and memory impairments in AD.
Differing Neurons in the Mammillary Body
The MIT team identified two different types of neurons in the mammillary body: lateral mammillary body neurons and medial mammillary body neurons. Compared to the medial neurons, in 5xFAD mice, lateral neurons exhibited more hyperactivity and higher expression of genes associated with synaptic activity.
Hypothesizing that lateral neurons may be more susceptible to AD, the team then compared lateral and medial MB neuron activity in 5xFAD mice and healthy mice. They observed that while there was no difference in the behavior of medial MB neurons, lateral MB neurons displayed higher levels of hyperactivity in the 5xFAD mouse model than in healthy mice. The researchers also observed that the hyperactivity in these neurons could be observed early (at two months of age for the mouse model, the equivalent of a young adult for humans) and, critically, even before the development of amyloid-beta plaques. Hyperactivity increased with age, and lateral MB neurons demonstrated more susceptibility to neurodegeneration than medial MB neurons with age.
The team found similar results in humans. Using single-cell RNA sequencing, the team studied postmortem human brain tissue samples from people with varying stages of AD. In doing so, they identified two distinct neural clusters corresponding to the lateral and medial MB neurons observed in mice. And just as with the mouse model, the team found signs of neural hyperactivity and neurodegeneration in the lateral MB neurons.
This could have significant implications for understanding AD progression. As Murdock explains, “We think the hyperactivity is related to dysfunction in memory circuits and is also related to a cellular progression that might lead to neuronal death.”
Future Treatment Options
Additionally, the team demonstrated potential avenues for future treatment options. The team treated the 5xFAD mice with levetiracetam, an epilepsy drug that treats seizures by reducing neuronal hyperactivity. The results were significant: the AD mouse model treated with the drug demonstrated significantly improved performance on memory tasks.
The specific vulnerabilities exhibited by lateral mammillary body neurons make them a promising target for the ongoing development of AD therapeutics. The study’s findings suggest that this brain region may contribute to the earliest symptoms of AD and may be a valuable area of future research focus.
For now, the team continues to work on understanding the connection between lateral MB neurons and other parts of the brain, particularly as it relates to memory formation and susceptibility to neurodegeneration.
Scantox is a part of Scantox, a GLP/GCP-compliant contract research organization (CRO) delivering the highest grade of Discovery, Regulatory Toxicology and CMC/Analytical services since 1977. Scantox focuses on preclinical studies related to central nervous system (CNS) diseases, rare diseases, and mental disorders. With highly predictive disease models available on site and unparalleled preclinical experience, Scantox can handle most CNS drug development needs for biopharmaceutical companies of all sizes. For more information about Scantox, visit www.scantox.com.