Huntington’s disease is a rare and fatal neurodegenerative disease caused by a genetic mutation that destroys brain cells in the basal ganglia, resulting in progressive motor, cognitive, and emotional impairments. Recent research breakthroughs out of MIT are shedding light on how this disease affects the striatum, a crucial part of the basal ganglia responsible for decision-making, emotions, and movement control. Researchers hope that this new understanding will lead to new treatment options for Huntington’s disease and other disorders that affect the striatum.
Huntington’s Disease Pathology
Huntington’s disease is an inherited, fatal, neurodegenerative disease caused by the expansion of an unstable repeat of CAG base triplets in the coding region of the Huntingtin gene, HTT. The primary pathology of Huntington’s involves the progressive loss of medium spiny neurons in the striatum. The loss of these neurons, which are involved in the indirect movement control pathway related to voluntary movements, leads to the motor dysfunctions, uncontrollable movements, and abnormal body postures associated with Huntington’s, along with psychiatric and cognitive impairments, and metabolic abnormalities.
Part of the basal ganglia, the striatum is responsible for making decisions that require evaluating the outcomes of a particular action. It is divided into striosomes, which are clusters of neurons, and the matrix, which surrounds the striosomes. This discovery was made decades ago by Ann Graybiel, MIT Institute Professor, member of MIT’s McGovern Institute for Brain Research, and one of the senior authors of the current study. Her work also revealed that striosomes are necessary for making decisions that require an anxiety-provoking cost-benefit analysis.
Additionally, we know from a 2007 study out of the University of Auckland that postmortem brain tissue from Huntington’s patients shows significant degeneration of the striosomes. That same 2007 study confirmed that while those patients were alive, they had demonstrated a number of mood disorder symptoms well before motor symptoms presented.
In a new study, Graybiel and other neuroscientists at MIT have furthered our understanding of how Huntington’s affects the cells in the striatum. For the first time, the MIT team of researchers were able to observe that two distinct cell populations in the striatum are affected differently by Huntington’s disease: the neurodegeneration of one of these populations leads to motor impairments, while damage to the other population may account for the mood disorders often seen in the early stages of the disease.
Striosomal Expression Patterns in Huntington’s
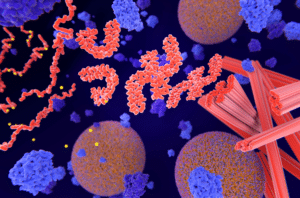
The team of researchers made this breakthrough observation by using single-cell RNA sequencing to analyze the gene expression patterns of striosomal and matrix cells. The team’s research utilized both human brain samples and brain tissue from two animal models of Huntington’s disease: the zQ175 transgenic mouse model and the R6/2 transgenic mouse model.
In their research, the team found that striosomal neurons are harder hit by Huntington’s than matrix neurons. More specifically, within the striosomes, D2 neurons (part of the “no go” pathway) are more vulnerable than D1 neurons (part of the “go” pathway). And the team observed that damage to the striosomes, which are known to be involved in regulating mood, may be responsible for the mood disorders that strike Huntington’s patients in the early stages of the disease, while later degeneration of the matrix neurons is what likely contributes to the decline of motor function that occurs later in the disease. Over time, the team found that these four major cell types begin to lose their identifying molecular identities and become more difficult to distinguish from one another.
The researchers hope their mapping of the striatum could lead to improved understanding of the many disorders that may be linked to the striatum, including Huntington’s disease, Parkinson’s, Autism Spectrum Disorder, obsessive-compulsive disorder, and Tourette’s.
The researchers also hope that better understanding of striosome damage in Huntington’s and related brain disorders could eventually lead to new treatments that target specific cells within the brain, with the ultimate goal of better treatments and outcomes for patients. As Graybiel summarizes, “There are many, many disorders that probably involve the striatum, and now, partly through transcriptomics, we’re working to understand how all of this could fit together.”
Scantox is a part of Scantox, a GLP/GCP-compliant contract research organization (CRO) delivering the highest grade of Discovery, Regulatory Toxicology and CMC/Analytical services since 1977. Scantox focuses on preclinical studies related to central nervous system (CNS) diseases, rare diseases, and mental disorders. With highly predictive disease models available on site and unparalleled preclinical experience, Scantox can handle most CNS drug development needs for biopharmaceutical companies of all sizes. For more information about Scantox, visit www.scantox.com.